How I Turned My Checkup Costs Into Tax Wins — Without the Headache
Paying for annual health checkups used to feel like a silent budget drain—until I discovered how smart tax planning could turn those expenses into savings. It wasn’t obvious at first, but medical costs, even routine ones, can unlock real financial benefits when handled right. I tested strategies, learned the rules, and wish I’d known sooner. This is how I stopped seeing medical checkup fees as just another bill and started using them as part of a smarter financial plan. What began as a personal experiment became a reliable system—simple, legal, and surprisingly effective. Now, every visit to the clinic carries not just health value, but financial potential.
The Hidden Cost of Ignoring Medical Expenses
For years, medical checkups were nothing more than a line item in the monthly budget—necessary, yes, but entirely one-sided. Like many, I viewed these payments as unavoidable losses, similar to utility bills or car maintenance. There was no thought of return, no sense of long-term benefit beyond physical well-being. Yet over time, the numbers added up. Annual blood panels, vision screenings, dental cleanings, and preventive imaging—each seemed small on its own, but together they represented hundreds, sometimes thousands, of dollars flowing out with no visible payoff.
What I didn’t realize then was that these expenses weren’t just health investments—they were also potential tax assets. In several tax systems, including those in countries with itemized medical deductions, qualified healthcare spending can reduce taxable income. But most people never claim them, either because they’re unaware, believe the threshold is too high, or assume only major treatments qualify. The result? A quiet but significant financial loss, repeated every year. This mindset—seeing medical costs solely as expenses—creates a blind spot in personal finance planning.
The true cost of ignoring this opportunity isn’t just missed savings; it’s the compounding effect of lost deductions over time. Imagine paying $800 annually for checkups across a decade—that’s $8,000 spent, yet if none of it is leveraged for tax relief, the full value remains unrealized. Worse, inflation and rising healthcare prices mean future costs will be even higher. Without a shift in perspective, families absorb these increases passively, treating them as inevitable rather than manageable. Recognizing that routine care can serve dual purposes—health protection and financial optimization—is the first step toward closing this gap.
What Qualifies? Decoding Eligible Medical Costs
Not every dollar spent on health counts toward tax benefits, which is why understanding eligibility is crucial. Broadly speaking, qualified medical expenses include amounts paid for the diagnosis, cure, mitigation, treatment, or prevention of disease. This encompasses a wide range of services that many consider part of standard preventive care. Routine physical exams, blood tests, mammograms, colonoscopies, vaccinations, and even certain screenings for cholesterol or diabetes often qualify. The key is that the service must be primarily for medical care, not general wellness or lifestyle improvement.
Many comprehensive health checkup packages offered by clinics include multiple components, some of which may qualify while others do not. For example, a full-body scan might include both diagnostic imaging (eligible) and optional nutritional counseling (possibly ineligible). Similarly, eye exams and vision tests are typically covered, but elective procedures like LASIK surgery may only qualify under specific conditions. Dental cleanings, X-rays, and fillings are usually accepted, whereas cosmetic dentistry such as teeth whitening does not count. The distinction lies in medical necessity versus personal preference.
Prescription medications and insulin are clearly eligible, but over-the-counter drugs generally are not—unless prescribed by a physician. This includes pain relievers, allergy medications, or supplements taken under medical supervision. Transportation costs to and from medical appointments can also be included, such as gas, parking, or public transit fares, provided they are directly related to receiving treatment. In some cases, lodging expenses for out-of-town medical visits may qualify if certain distance and duration criteria are met.
It’s important to note that insurance reimbursements affect deductibility. If a portion of the expense is covered by insurance or a health savings account (HSA), only the out-of-pocket amount can be claimed. For instance, if a $300 lab test is partially reimbursed with $200 from an HSA, the remaining $100 becomes the eligible figure. Keeping detailed records of payments and reimbursements ensures accurate reporting and prevents double-counting, which could raise red flags during an audit. Understanding these boundaries helps individuals make informed decisions about what to include and how to structure their claims effectively.
Why Tax Planning Beats Last-Minute Panic
Filing season often brings a rush of last-minute decisions, especially when it comes to medical deductions. Many wait until March or April to gather receipts, only to find that critical documents are missing, dates are unclear, or expenses were never tracked systematically. This reactive approach not only increases stress but also reduces the likelihood of maximizing legitimate claims. By then, opportunities to adjust spending or bundle services for greater impact have already passed. Waiting until the deadline turns tax planning into damage control rather than strategic optimization.
In contrast, proactive tax planning integrates medical expenses into the broader financial calendar. This means thinking ahead about when to schedule procedures, how much to expect in out-of-pocket costs, and whether combining certain visits within a single tax year could push total eligible expenses over the deduction threshold. In systems where medical deductions are subject to a percentage of adjusted gross income (AGI), such as 7.5% in some frameworks, every additional dollar above that floor increases tax savings. Planning allows individuals to aim for that threshold intentionally, rather than hoping it happens by chance.
Another advantage of early planning is the ability to coordinate with other financial activities. For example, someone considering elective medical procedures—like joint evaluations or cardiac screenings—can time them to coincide with years of higher income or anticipated deductions. This alignment improves overall tax efficiency. Likewise, families expecting changes in insurance coverage can use the transition period to front-load necessary tests before deductibles reset. These decisions require foresight, not urgency.
Moreover, integrating health and financial planning fosters better budgeting habits. When medical spending is viewed through a dual lens—health outcome and tax impact—households tend to track it more carefully. They become more aware of costs, compare providers, and seek value. This leads not only to smarter healthcare choices but also to improved financial discipline. Instead of treating medical bills as random shocks, families begin to anticipate them, prepare for them, and even use them to their advantage. That shift—from passive acceptance to active management—is where real financial progress begins.
Smart Timing: Syncing Health Checks With Tax Strategy
The timing of medical appointments can significantly influence tax outcomes, even when the total annual spending remains unchanged. Consider this scenario: a person has already incurred $3,000 in eligible medical expenses in one tax year, but the deduction threshold is $3,500 based on their AGI. An additional $600 in checkup costs could make the entire $3,600 deductible. If those tests are scheduled early in the next calendar year, the benefit is lost. But if they’re moved forward by a few weeks—into the current year—the full amount becomes claimable. That simple shift could result in hundreds of dollars in tax savings.
This principle applies broadly. Bundling routine services within a single tax year allows individuals to concentrate expenses strategically. For example, scheduling both a dental deep cleaning and a follow-up periodontal evaluation in December instead of splitting them across two years can help cross the deduction threshold more efficiently. The same logic works for vision care—getting new prescription glasses and a comprehensive eye exam in the same period increases the claimable total. None of these actions increase actual spending; they simply reorganize timing for maximum financial benefit.
Front-loading is another effective tactic. If a doctor recommends annual screenings, there’s often flexibility in when they’re conducted. Moving a blood panel or bone density scan from January to late December allows it to count toward the current year’s total. This is especially useful in years when medical spending has been low due to good health. By accelerating planned procedures, individuals can avoid leaving potential deductions on the table.
Similarly, delaying non-urgent tests can be advantageous in certain situations. If someone has already exceeded the deduction threshold in the current year, pushing a minor screening into the next year preserves the expense for future use. This creates a kind of “tax savings reserve” that can be tapped when medical costs are lower. It’s a balancing act—knowing when to pull expenses forward and when to hold them back—but one that pays off over time. With a little coordination between the calendar and the checkbook, ordinary healthcare decisions become tools for smarter financial management.
Record-Keeping Hacks That Actually Work
Even the most strategic tax planning fails without proper documentation. A receipt buried in a glove compartment or a faded email receipt lost in an inbox does no good come filing time. Yet many people avoid organized record-keeping because they assume it requires complex software, digital expertise, or hours of weekly maintenance. The truth is, effective systems don’t need to be high-tech—they just need to be consistent and accessible.
One practical method is the dedicated medical expense folder—a simple, labeled binder kept at home. Every time a payment is made, the receipt, invoice, or statement is printed and placed inside, sorted by date. Alongside each document, a brief note can be added: the type of service, the provider, and the out-of-pocket amount. This physical system works especially well for those who prefer tangible organization and want immediate access during tax season. It also serves as a visual reminder of how expenses accumulate over time.
For those comfortable with digital tools, a smartphone photo system is highly effective. After any medical visit, take a clear picture of the receipt or payment confirmation and save it in a labeled folder such as “Medical Expenses 2024.” Cloud storage services like Google Drive or iCloud automatically back up these images, reducing the risk of loss. Some users even create a spreadsheet to log each transaction—date, provider, service type, and cost—which can later be sorted and totaled for reporting purposes. The key is to do it immediately, not weeks later when memory fades.
Another overlooked but valuable source of records is the Explanation of Benefits (EOB) form sent by insurance companies. While not a payment receipt, it details what was billed, what was covered, and what remains the patient’s responsibility. Keeping EOBs alongside actual payment proofs ensures a complete picture of each expense. When combined with bank or credit card statements—highlighted to show medical transactions—this creates a layered, audit-ready file. The goal isn’t perfection, but clarity and consistency. With a reliable system in place, gathering tax documents becomes routine, not stressful.
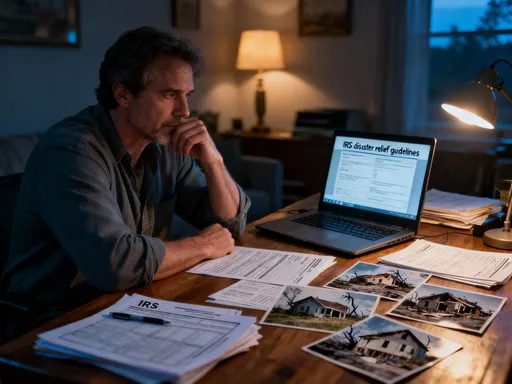
When to Seek Help: Knowing Your Limits
While many households can manage medical expense claims on their own, there are situations where professional guidance makes sense. Tax laws are not static—they evolve, and interpretations can vary. A rule that applied last year may have changed, or a seemingly straightforward expense might have complex implications due to insurance structure, dependents, or cross-border care. Recognizing when to consult a tax advisor isn’t a sign of failure; it’s a sign of responsible financial management.
One red flag is unusually complex billing. Some clinics provide itemized invoices with dozens of line items, mixed codes, and partial reimbursements. Sorting through these requires time and knowledge of medical coding conventions. If the breakdown is unclear or if services span multiple categories—some eligible, others not—expert review can prevent errors and ensure accurate claims. Similarly, families with multiple dependents or shared healthcare accounts may struggle to allocate expenses correctly across filers. A professional can clarify ownership and optimize who claims what.
Cross-border medical treatment introduces another layer of complexity. If care was received in another country, eligibility rules may differ, and currency conversion, documentation standards, and foreign tax credits come into play. While occasional international visits for checkups are becoming more common, especially in regions with specialized clinics, the tax treatment of such expenses is not always straightforward. In these cases, advice from a qualified tax professional familiar with international regulations can prevent costly mistakes.
Another scenario calling for help is when medical expenses are exceptionally high—perhaps due to chronic conditions or major procedures. While this increases the likelihood of qualifying for deductions, it also raises the chance of scrutiny during an audit. A tax advisor can help structure the claim properly, ensure all supporting documents are in order, and provide representation if needed. The cost of professional help should be weighed against potential savings and peace of mind. Often, even a single consultation at key moments—such as before filing or after a major health event—can yield long-term benefits.
Building a Health-Financial Habit That Lasts
Sustainable financial health doesn’t come from one-time wins, but from consistent, repeatable habits. Turning medical checkup costs into tax advantages should not be a one-off experiment, but an integrated part of annual financial life. The goal is to make this process automatic—so natural that it requires little extra effort each year. Like setting a calendar reminder for a flu shot, families can build triggers that prompt both health and financial actions simultaneously.
Start by aligning the annual checkup with the fiscal calendar. Choose a consistent time of year—such as spring or fall—to schedule comprehensive screenings. Mark this date not only on the family planner but also in the financial calendar. Use the same occasion to review last year’s medical spending, update records, and assess whether the previous tax claim was optimized. This dual-purpose ritual reinforces the connection between health and finance.
Next, incorporate medical budgeting into the household’s annual financial review. Just as you plan for property taxes, car maintenance, or vacation costs, include an estimate for out-of-pocket healthcare. Track actual spending against this forecast throughout the year. If spending runs low, consider whether any recommended screenings can be moved up to maximize future deductions. If it runs high, verify that all eligible expenses are being documented. This ongoing awareness supports better decision-making and reduces year-end surprises.
Finally, use technology to reinforce consistency. Set recurring reminders on a phone or calendar app to gather receipts monthly, review insurance statements quarterly, and back up digital files annually. Link these tasks to existing routines—like paying bills or grocery shopping—to increase follow-through. Over time, these small actions compound into a resilient system. What once felt like extra work becomes second nature. And in that shift lies the real victory: not just saving money on taxes, but transforming routine healthcare into a pillar of long-term financial well-being.